TMJ Syndrome
What is TMJ Syndrome?
The temporomandibular joint (TMJ) is where your jaw attaches to the skull. It is a hinge type joint that allows for opening and closing and side to side movement of your mouth. When this joint and/or the musculature around it become irritated or stops working properly, you can develop Temporomandibular Dysfunction (TMD). There is one joint on each side of the skull. Therefore, TMD can occur on just one side or both.
TMJ Anatomy
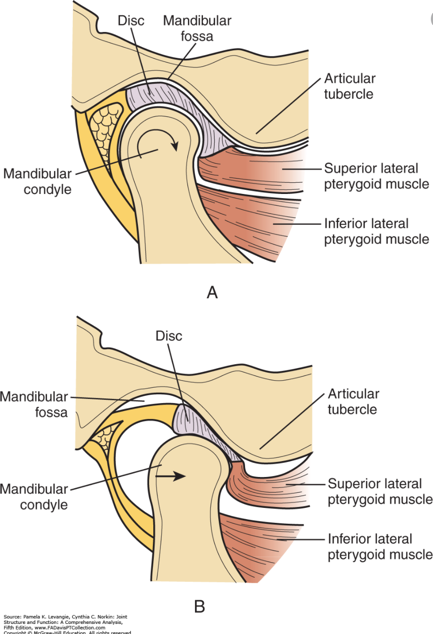
The mandible (Jaw bone), and temporal bone form the TMJ. Between these two bones sits an articular disc (cushion), which attaches to the joint capsule and musculature anteriorly and the retrodiscal tissue posteriorly. The retrodiscal tissue has blood and nerve supply, unlike the rest of the disc, and therefore often contributes to pain.
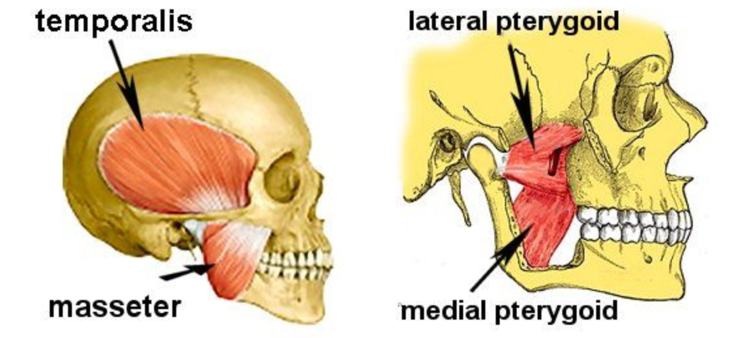
The muscles of mastication (temporalis, masseter, lateral pterygoid, and medial pterygoid) assist with the movement of the jaw. The temporalis, masseter, and medial pterygoid work to elevate the jaw, while the lateral pterygoid aids in protraction of the mandible, depression of the chin, and lateral deviation of the mandible.
Risk Factors for TMJ Syndrome
- Trauma or injury to the jaw
- Arthritis
- Clinching or grinding teeth
- Stress
- Malocclusion (poor alignment of the teeth)
- Lockjaw
- Disc displacement (displacement of the cushion between the mandible and temporal bone)
- Lifestyle or occupation that involves prolonged sitting with poor posture
- Dental surgery
- Infection.
There is some research to support that TMD is more common in women than men and is more likely to affect individuals between the ages of 20 to 40.
Signs & Symptoms of TMJ Syndrome
- Inability to open mouth
- Clicking and popping with an opening (may or may not be painful)
- Pain in jaw, face, or neck
- A jaw that gets “Locked”
- Facial swelling
- Difficulty chewing
- The sensation that teeth are not aligned
- Headache
- Earache or “Fullness” in-ear
- Dizziness
- Tinnitus (ringing in ears)
TMJ Syndrome Diagnoses
Most individuals first seek out treatment from their dentist due to the location of the pain. During the history, your dentist may ask if you have been told that you grind your teeth at night, if you have ever had your mouth get “Stuck open or closed,” or if you have noticed any popping or clicking with the movement of the jaw. During the physical exam, your dentist will feel the muscles of your jaw, check the joint for abnormalities, and feel for clicking and popping. Your dentist will also assess your bite to ensure proper alignment of your teeth. An x-ray may be ordered to rule out other pathologies, such as, infection and, in some cases, further imagining may be done to assess the joint and disc. From there, many dentists refer to a specialist such as an oral surgeon or facial pain specialist. You may also be referred to an ENT to rule out serious pathology depending on your symptoms.
In mild cases of TMD, it is recommended that you take over the counter NSAIDs, eat soft foods, alternate cold, and hot compresses, and avoid max opening until your symptoms resolve. If your dentist is concerned about grinding and clenching, you may be prescribed an oral orthotic (night guard).
How can a Physical Therapist Help with a TMJ Syndrome?
If you have persistent pain and TMD, you will be referred to a physical therapist for treatment. Your physical therapist will take a subjective history similar to your dentist with the addition of questions about occupational habits, postural habits, headaches and dizziness, history of neck pain, and exacerbating and relieving factors. A thorough physical exam will be completed to assess a range of motion and deviation with opening and closing of the mouth and lateral movement of the jaw. Your physical therapist will also perform intra (inside) oral and extra (outside) oral palpation for muscle tightness and guarding in the muscles of mastication and feel for popping and clicking with jaw movements. Neck range of motion, sitting posture, and neck and scapular musculature will be assessed to determine if these areas are contributing to pain. Once your evaluation is complete, you and your physical therapist with discuss your individualized treatment plan and goals.
Typical treatment for TMD includes manual therapy, postural strengthening, postural education, and stress reduction. Manual therapy is performed intra (inside) orally and extra (outside) orally to decrease muscle tightness and guarding in the muscles of mastication. Patients can be taught to perform muscle release intra (inside) orally and extra (outside) orally at home if comfortable. Postural strengthening will focus on the neck and upper back to decrease strain on the TMJ related to poor posture and positioning. Postural awareness is important especially for those that have jobs that require prolonged sitting. Your physical therapist will discuss good sitting and mobility habits as well as jaw relaxation exercises. If you have a “desk job”, your physical therapy will discuss proper workplace set up and ergonomics in order to decrease strain on your neck and TMJ. Stress reduction is important to decrease unintentional clenching and tightness in the muscles of mastication. Techniques like meditation, regular exercise, deep breathing, and yoga can all be used to better manage stress.
For more information check out the following sites:
https://www.mouthhealthy.org/en/az-topics/t/tmj – American Dental Association
https://www.nidcr.nih.gov/health-info/tmj/more-info – National Institute of Dental and Craniofacial Research
https://www.choosept.com/symptomsconditionsdetail/physical-therapy-guide-to-temporomandibular-joint-disorder – American Physical Therapy Association





