Smith Fracture
What is a Smith Fracture?
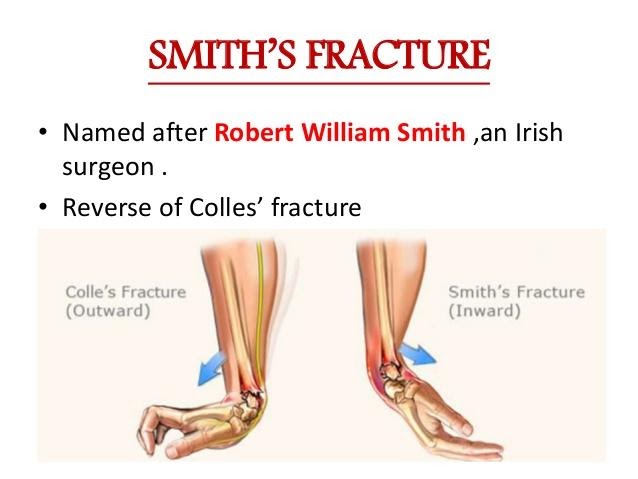
A Smith fracture is a fracture of the distal radius that is caused by direct trauma to the back of the wrist or from falling on a flexed wrist. The radius is the larger of the two forearm bones and the distal end is the portion closest to the wrist and hand. This injury results in the palmar displacement of the distal part of the joint, meaning that the bone will fracture at the end closest to the hand and the fractured portion of bone will move forward toward the palm. Smith fractures are relatively rare and account for less than 3% of all radius fractures. They most often occur in young males (high energy falls) or older females (osteoporosis).
Smith fractures are categorized into three types:
- Type I is an extra-articular (does not extend into the joint) transverse (perpendicular) fracture through the distal radius and is most common (~85% of cases)
- Type II is an intra-articular (extends into the joint) oblique (diagonal) fracture of the distal radius and is less common (~13% of cases). Type II Smith fractures are also called reverse Barton fractures.
- Type III is a juxta-articular (near joint) oblique fracture of the distal radius and is very uncommon (less than 2%).
How is a Smith Fracture Diagnosed?
A plain film radiograph (x-ray) is typically used to formally diagnose Smith’s fractures. Signs and symptoms of a Smith fracture generally include immediate pain and swelling, bruising, and tenderness, as well as decreased range of motion and strength. If the fracture is severe, the wrist may hang or be positioned in an unusual way, but if the fracture is not severe the individual may be able to functionally use the wrist with pain. Evaluation of the involved upper extremity’s nerves will be performed to rule out any issues. In some cases, individuals may experience compression of the median nerve in the Carpal Tunnel at the front of the wrist or may experience compression of the radial or ulnar nerves.
Immediate care following a Smith fracture will be carried out by an orthopedist and will consist of realigning the broken bones in order to promote healing. Smith fractures can usually be treated with closed reduction (moved back into place) and casting in extension, but surgical fixation is required in cases where the fracture remains unstable following reduction, or in cases with nerve involvement.
How can a Physical Therapist Help with a Smith Fracture?
Treatment in regard to therapy following reduction will vary based on the individual’s age, the extent of the fracture, and the activity level. In general, individuals will wear a cast for approximately 6 weeks and will then undergo physical or occupational therapy to return to a prior level of activity.
Physical or Occupational therapy for a Smith fracture may include:
- Passive and active range of motion focusing on wrist flexion/extension and forearm supination
- Isometric strengthening
- Possible splinting
- Progressive strengthening and stabilization of the upper extremity as mobility improves
- Grip strengthening
- Weight-bearing exercise through the arm (such as wall push-ups, or quadruped exercises)
- Specific functional strengthening and work-related tasks
- Joint mobilizations if minimal improvement
Prompt and proper treatment of Smith fractures is imperative to ensure correct bone healing and to regain the full function of the wrist and hand. Individuals with closed reduction generally have good outcomes and usually have evidence of functional healing after 6 weeks. Those who have to undergo surgical fixation generally have a longer rehabilitation process and full recovery usually takes about a year.
For More Information:



