Hip Osteoarthritis
What is Hip Osteoarthritis?
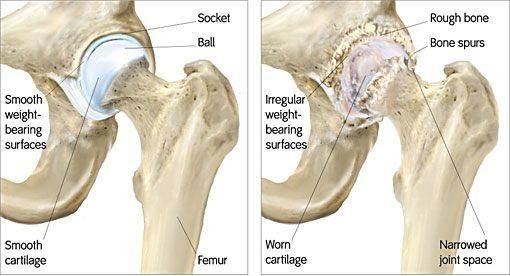
Osteoarthritis (OA) is a degenerative joint disease that occurs most often in weight-bearing joints. The most common form of (OA) is primary, meaning that it occurs without an injury and typically progresses throughout your lifetime. As we age, the cartilage that typically protects our joints is damaged and erodes. As this protective covering is damaged, the bones in the joint start compressing each other- causing inflammation, pain, and damage to the bones. However, other disease processes (ex. Obesity or metabolic disorders), joint injuries, or occupational risk factors can also increase your risk of Hip Osteoarthritis.
- Important anatomy of the hip:
- Bones: The hip joint is formed by the acetabulum of the pelvis and the head of the femur; both are covered with articular cartilage and synovial fluid. The cartilage functions as a protective cover to cushion your joints and the synovial fluid allows for the joint to move without friction.
- Ligaments: The hip joint is made strong and stable with many ligaments, which their primary function is to provide stability to the joint.
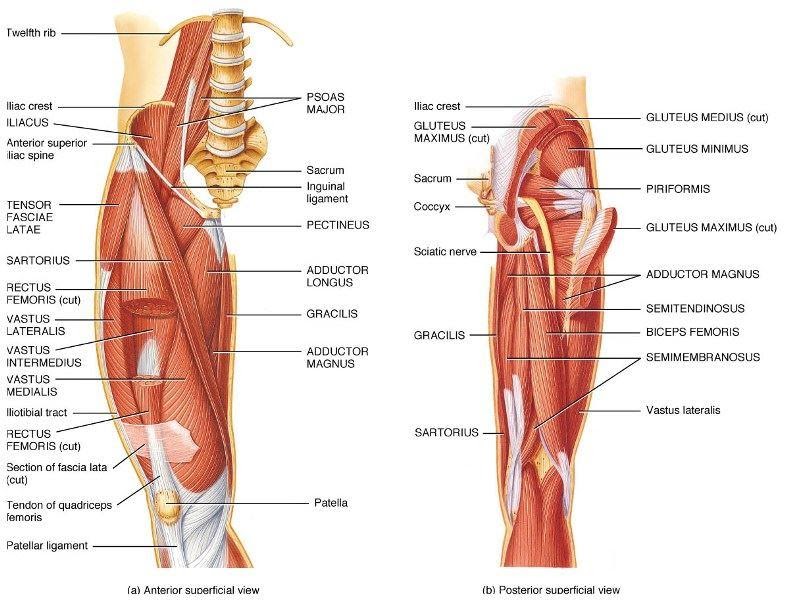
- Muscles: Muscles are not only essential for movement; they also provide hip joint stability and limit unnecessary forces on our joints. The big muscle groups in our hips are: Hip flexors (Iliopsoas, rectus femoris); Hip extensors (Gluteus maximus, hamstrings), Hip external rotators (gluteus maximus, piriformis), Hip internal rotators (gluteus minimus, tensor fascia latae), Hip abductors (gluteus medius, tensor fascia latae), & Hip adductors (adductors, gracilis, and pectineus).
How is Hip Osteoarthritis Diagnosed?
- Patient’s Symptoms: The primary complaint with OA is progressive pain and stiffness that is worst in the morning and then increases with activity. People with OA report increased difficulty doing their normal daily activities and inability to participate in their recreational activities due to pain. Other patient-reported symptoms include swelling or tenderness around the hip joint, pain in the groin, catching/locking of the hip, changes in their gait, crepitus (Popping/grinding in joint with movement), and loss of flexibility (Range of motion).
- Examination: In addition to the subjective patient reports; a physical examination and diagnostic imaging will be performed to get an official diagnosis. Prior to taking any images of the hip, a physical examination will be performed- measuring the strength of hip muscles, hip range of motion (An early sign can be limited abduction and rotation), placing pressure on the hip joint in various positions to determine if the pain is coming from the hip joint or other areas around the hip.
Radiographs (x-rays) are usually the first imaging done and this can show a narrowing of the joint space, which indicates a loss of the protective cartilage and synovial fluid. This will also show any bone spurs and changes in the bony structure of the hip joint. MRI can also be done but is not always needed unless more in-depth images are needed.
How Can Physical Therapy Help with Hip Osteoarthritis?
Exercise of all forms have been shown to help improve pain, flexibility, and overall mobility in people with hip OA. Even though physical therapy (PT) cannot change the boney changes that have occurred in the hip, PT can help improve some of the contributing factors (Muscle weakness and flexibility) in order to reduce pain and making it easier to get around.
Depending on the pain and level of restriction in your everyday life, surgery may be required. Typically, a total hip replacement is performed to replace the diseased bone with artificial implants. Even if surgery is the ultimate path, PT can still help you before and after the surgery. Preparing for surgery can help improve your strength and motion in your painful hip to either prolong the need for surgery or to facilitate a quicker recovery after surgery. When considering surgery- remember that you are going to be weaker afterwards, so the stronger you go in, the better you will be afterwards.
No matter what goals you have for attending PT, here at Kinetic, we want to work with you to achieve your goals. After your initial evaluation, we will personally tailor each treatment to your individual needs. Whether we are working on strengthening, flexibility, balance, or even working in our pool, we will use all our resources to get you back on track or where you want to go. You will be working 1-on-1 with a physical therapist who truly treats you as a whole and not just your hip.