Spina Bifida
What is Spina Bifida?
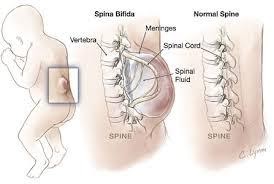
The anatomy of the affected area in Spina Bifida includes the spinal cord and the nerves. The spinal cord provides a communication pathway from the brain to and from the various parts of the body for movement, sensation, and operation. The nerves provide communication.
Factors Placing People at Heightened Risk for Spina Bifida:
- Folate deficiency (a natural form of vitamin B-9)
- Family history of neural tube defects
- Some medications, including anti-seizure drugs
- Diabetes
- Obesity
- Increased body temperature during early pregnancy, which can happen due to excess heat exposure or fever
- For many children, the causes is not known.
How Is Spina Bifida Diagnosed?
Spina bifida can often be found by a routine ultrasound between 16 to 18 weeks. If no skin covers the defect, abnormally high alpha-fetoprotein (AFP) levels in the blood and amniotic fluid support a diagnosis. Other methods of diagnosis include; high-resolution ultrasound, ultra-fast fetal MRI, fetal echocardiogram, amniocentesis, and a maternal serum alpha-fetoprotein (MSAFP) test.
Symptoms and Associated Conditions of Spina Bifida
The symptoms may vary depending on which type of spina bifida is present and the following: the size and location of the neural tube defect, whether skin covers the affected area, and which spinal nerves are exposed. They can range from mild to severe.
- Walking and mobility problems, including weakness and paralysis
- Orthopedic complications, including scoliosis (curved spine), abnormal growth, dislocation of the hip, bone and joint deformities, and muscle contractures
- Bowel and bladder control problems
- Hydrocephalus (accumulation of fluid in the brain)
- Chiari Malformation Type II, which can cause breathing and swallowing dysfunction
- Meningitis, infection in the tissue surrounding the brain, which can cause brain damage
- The tethered spinal cord, which can affect the function of the legs, bowels, and bladder
- Sleep apnea or other sleep disorders
- Higher susceptibility to incurring wounds and skin problems due to decreased sensation
- Learning disabilities
- Gastrointestinal problems
- Depression
How can a Physical Therapist Help with a Spina Bifida?
An Occupational therapist can help your child with spina bifida in many ways. An OT can provide training on how to complete daily activities within the child’s ability level, assess and provide treatment for symptoms present, such as weakness, decreased use of limbs, and decreased independence in daily routine. They can help your child develop motor milestones, issue adaptive equipment if needed, complete a wheelchair examination in order to get your child the appropriate wheelchair and other positioning devices, make or recommend braces in order to prevent further contracture (tightening of muscles), and help with other equipment your child may need, such as a bath chair or adaptive car seat. They can aid you in pressure management techniques and equipment. They can also help with the development of the hand and arm skills, dressing, bathing, self-feeding, play skills, and other daily living skills. Finally, they can help in developing learning skills, which may be affected if your child presents with a learning disability affecting attention or ability to complete tasks.





