Patellofemoral Syndrome (PFPS)
What is Patellofemoral Syndrome (PFPS)?
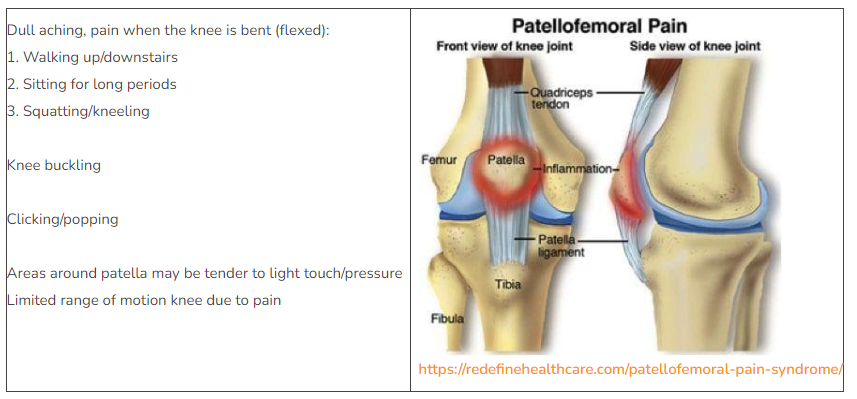
Patellofemoral pain syndrome (PFPS), also known as “Runner’s knee,” is an umbrella term for pain at and around the front of the knee. It can include the patellofemoral joint and/or surrounding soft tissues. The patellofemoral joint is the space at the front of the knee where the patella (knee cap) meets the femur (Thigh bone). The underside of the patella and end of the femur are covered with cartilage. The patella glides in a groove of the femur with the assist of the quadriceps and patellar tendons whenever the knee is bent or straightened (see image). If any of these surrounding structures are too tight, too loose, weak, or injured, the patella will not glide in its natural path, causing it to rub against the femur. This rubbing can cause irritation, inflammation, and wearing away of the cartilage between the patella and femur.
Causes – overuse, weakness of surrounding muscles at knee and hip, injury/trauma to the kneecap (Fracture, dislocation, etc.), poor mechanics of the foot with weight-bearing activities, post-surgical
Risk factors – age (Commonly seen in adolescents and young adults), sex (More common in women than men and attributed to the wider pelvis which alters the angle at which the bones of the knee joint meet), certain sports/activities (Running/jumping sports increase stress on knee)
Signs & Symptoms of Patellofemoral Syndrome (PFPS)
Diagnosis of Patellofemoral Syndrome (PFPS)
PFPS is a diagnosis of exclusion, which means a clinician will assess for other knee conditions to rule out other pathologies with similar signs and symptoms. A physical examination usually can diagnose patellofemoral pain syndrome, but a physician may order an X-ray to rule out damage to the knee and its surrounding tissues.
How can a Physical Therapist Help with Patellofemoral Syndrome (PFPS)?
Exam
The primary goal of therapy for PFPS is to relieve pain and restore range of motion and strength. This condition can commonly be treated non-surgically. A clinician will discuss your symptoms including when the pain started, the severity of pain, and a description of pain. The clinician will also need to know what activities cause or increase pain. You may be asked to perform activities such as climbing stairs, jumping, or squatting during the exam for assessment of strength and body mechanics. The examination will also include a range of motion at the knee and its surrounding joints, palpation of the surrounding muscles, ligaments, and tendons, the strength of the surrounding muscles, the flexibility of soft tissues throughout the limb, and an assessment of the way you walk.
What do my feet and hips have to do with my knee?

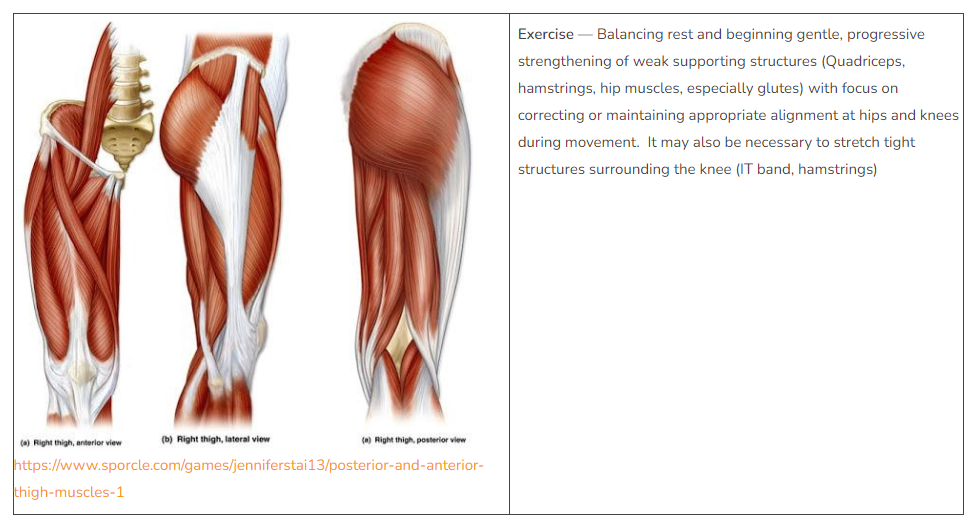
Several muscles and tendons that control the movement of the knee also assist with movement at the hip or ankle. Therefore, strengthening the muscles above and below the knee will affect mechanics at the knee. Strengthening of hip muscles, particularly the glutes can improve the alignment of the patella during movement and reduce pain at the knee. The improvement of strength at the hip will improve proprioception (awareness of position and movement of the body) and control at the knee.
Because the knee joint includes the femur (thigh bone), patella (kneecap) and tibia (shin bone), rotation at the foot/ankle will affect the alignment of the patella within the knee joint. For example, during weight-bearing activities (standing, walking, squatting), if the arch tends to collapse (pronate) then the tibia will rotate inward which will change the overall positioning of the knee. Strengthening at the foot and ankle can improve the arch response to the ground during weight-bearing, maintain the correct position of the patella in the groove of the femur and decrease pain with activities requiring knee flexion.
Treatment for Patellofemoral Syndrome (PFPS)
Taping/bracing may be utilized to provide external support to the patella for correct tracking with knee flexion. Tape may also be used to improve proprioception during movement to make a person more aware of what is happening at the affected limb and improvement conscious control of movement.
Orthotics may be recommended for proper foot positioning during weight-bearing activities. Shoe inserts can help improve the alignment of the foot and ankle, which will decrease forces that are absorbed through the lower leg.
Low impact activities – cycling, swimming, biking
Ice and NSAIDs
For more info
References:
https://www.physio-pedia.com/Patellofemoral_Pain_Syndrome
https://www.medbridgeeducation.com/patient-education-library/condition/95-Patellofemoral-Pain
https://orthoinfo.aaos.org/en/diseases–conditions/patellofemoral-pain-syndrome/





