Colles Fracture
What is a Colles Fracture?
This fracture occurs in patients of all ages, but is more prevalent in the pediatric/young athletic, and elderly populations who are susceptible to falls given higher activity level/risky behavior in the former group and poorer balance related to ageing in the latter group. Interestingly, men are more likely to experience a Colles fracture in their youth, while women are more likely to sustain this fracture as they age (Amplified by increased prevalence of osteoporosis among this ageing population).
How is a Colles Fracture Diagnosed?
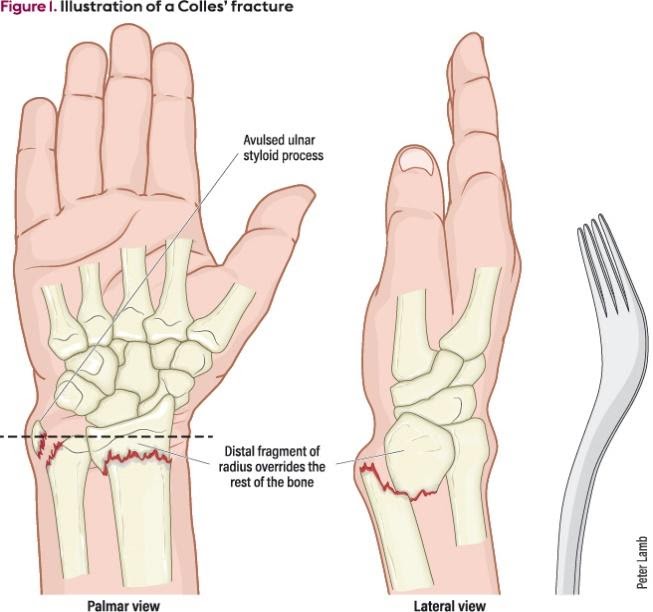
Given that this injury is associated with trauma, imaging should be a part of the initial evaluation. An orthopedist will likely order for a radiograph first, including PA (Posterior-anterior), and lateral views, and a “CT- scan” might be ordered if the injury needs more precise visualization for an accurate diagnosis. In addition to imaging, the patient will commonly present as a painful extension deformity at the wrist “dinner-fork deformity” with bruising, swelling, decreased range of motion at the wrist and forearm, and poor grip of strength. The patient should be assessed for neurovascular (Nerve and blood vessel) function of the wrist and hand as he or she may present with altered pulses, sensation, and motor function related to the fracture.
The severity of the fracture will determine if it is treated conservatively (Non-operative), or surgically. Most of these fractures are treated conservatively with closed reduction the physician will manually correct the deformity by applying a palmar and medially directed force to the distal radial fractured segment, while maintaining traction at the hand and counter traction at the elbow), and immediate splinting followed by casting for 6-8 weeks. If the fracture is unstable or severely displaced, surgery will be the preferred option in order to maximize function and limit post-injury complications such as mal-union (Poor healing), non-union (non-healing), and severe radial shortening that will increase loading through the ulna on the inside of the forearm.
How can a Therapist Help with a Colles Fracture?
A physical or occupational therapist will be involved in the patient’s care early-on following either reduction with casting or surgical repair immediately following the injury. The therapist may only see the patient occasionally during the early immobilization stage in order to provide:
- Edema management
- Inspection for red-flag signs/symptoms including discoloration of fingers/nail beds, or numbness/tingling of the fingers
- Education for movement of non-involved joints (Specifically at the distal hand with tendon gliding and intrinsic muscle exercises)
The patient will be seen more frequently once the immediate immobilization period has ended, which will vary based on the orthopedist. In general, wrist motion can begin as early as 3 weeks postoperatively with ORIF (open reduction and internal fixation) or at 6-8 weeks after external fixation or closed reduction with immobilization. During this phase, the emphasis will be on a range of motion of the wrist, forearm, and elbow, progressing as follows:
- Passive range of motion performed by the therapist
- Active-assisted (opposite hand-assisted) range of motion
- Gravity-assisted range of motion
- Full active range of motion based on patient’s tolerance and response to treatment
The later stages of rehab will focus more on function:
- Wrist and hand (as well as general upper extremity) strength and endurance
- Return-to-work activities






