Guide to Understanding Your Insurance plan
Insurance Plan 101 for Physical Therapy Patients
So, your insurance plan “covers” physical therapy or occupational or speech therapy—which means you won’t have to pay anything out-of-pocket for your therapy visits, right? Not quite. The fact that your insurance plan covers physical therapy services—or any other services, for that matter—doesn’t necessarily mean you’re off the hook as far as payment goes. In many cases, you’ll still have to pay a deductible, a co-insurance, or a copayment. Talk about tricky.
To better understand the terms of your insurance plan, you first must understand the terminology. Here are a few common questions regarding insurance lingo:
This is the total amount you must pay out-of-pocket before your insurance starts to pay. For example, if your deductible is $1,000, then your insurance won’t pay anything until you have paid $1,000 for services subject to the deductible (keep in mind that the deductible may not apply to every service you pay for). Furthermore, even after you’ve met your deductible, you may still owe a copay or co-insurance for each visit.
This is a fixed amount that you must pay for a covered service, as defined by your health plan. Copays usually vary for different plans and types of services. Typically, you must pay this amount at the time of service. Again, copay amounts are fixed—which means you will always pay the same amount, regardless of visit length. In most cases, copayments go toward your deductible.
This type of out-of-pocket payment is calculated as a percent of the total allowed amount for a particular service. In other words, it’s your share of the total cost. For example, let’s say:
- Your insurance plan’s allowed amount for an office visit is $100.
- You’ve already met your deductible.
- You’re responsible for a 20% coinsurance.
In this situation, you’d pay $20 at the point of service. The insurance company would then pay the rest of the allowed amount for that visit. Keep in mind that the coinsurance amount may vary from visit to visit depending on what services you receive.
Medicare Part B patients are responsible for a 20% coinsurance, which typically amounts to approximately $25 per visit. If you have original Medicare as your primary insurance, but you also have a secondary insurance, the secondary payer becomes responsible for the 20%. In some cases, the secondary insurance also charges a copay, coinsurance, or deductible. We recommend contacting your secondary insurance carrier to find out.
If you have not yet met your deductible, then you will pay $120 for your initial evaluation visit for physical or occupational therapy and $85 per follow up visit. We charge coinsurances based on the estimate of what your insurance covers. On average if you have a 20% coinsurance, you’ll pay $25; if you have a 10% coinsurance, you’ll pay $15. You’ll then owe any applicable coinsurance balances after we receive the Explanation of Benefits (EOB) from your insurance company. Conversely, if we find that you have overpaid, we will refund you via check as soon as possible. As for copayments—these amounts rarely vary, so if your copay for physical therapy visits is $25, your insurance requires you to pay that $25 at each visit.
Your health is our number-one priority. As such, we have a partnership with Care Credit to provide low cost financing options to fit your needs.
Examples of EOBs for Physical Therapy Services
Here are a few examples of Explanations of Benefits (EOBs) for physical therapy services. An EOB is a document your insurance plan sends to explain the various costs—including the amount you, as the patient, are responsible for—associated with your care. For definitions of the terms included in these examples, skip down to the bottom section of the page.
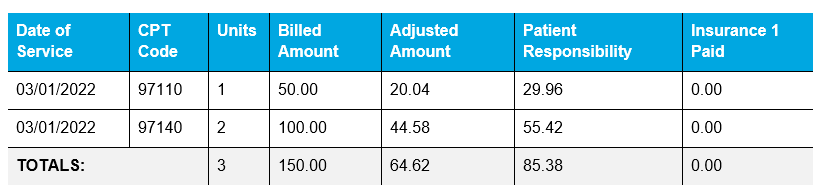
Insurance 1: Patient has not yet met his or her annual deductible. Therefore, the patient is responsible for 100% of the allowed amount.
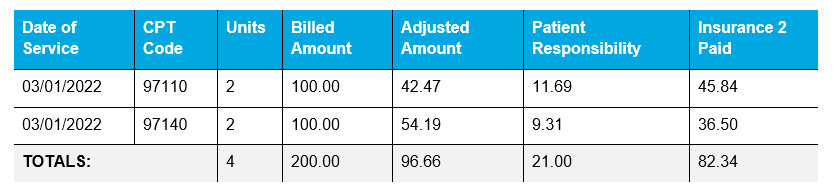
Insurance 2: Patient owes a 20% coinsurance for PT services.
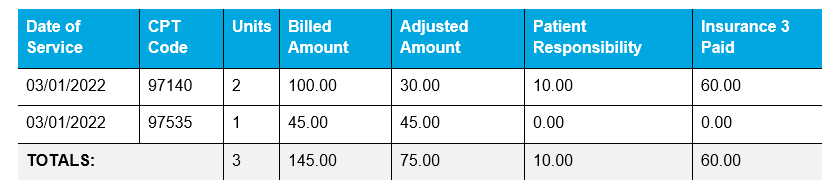
Insurance 3: Patient owes a $10 copay for PT visits.
Insurance Plan Definitions
The date of your visit.
The code denoting each service provided to you during your visit (e.g., manual therapy, therapeutic exercise, self-care instruction, aquatic therapy, etc.). You can request a list of these codes—along with their explanations—from your insurance company.
This is the amount we billed the insurance company for that particular service. The billed amount may vary depending on the duration of the service, the facility in which the service was provided, or the state in which the facility is located.
This amount is not a payment, but rather a write-off or “reduction.” It is based on the contract in place between your provider (us) and your insurance company. Neither you nor the insurance company pays this amount. The provider essentially writes it off (which is why it is sometimes called the provider’s responsibility).
This column may be labeled “Deductible,” “Copay,” “Coinsurance,” or “Patient Pay.” It is the amount that you, the patient, are responsible for paying. If a secondary insurance is on file, we will forward this amount to that insurance for payment. Once we get the secondary EOB back, you will receive a bill for any outstanding balances in the patient responsibility column.
This is the amount the insurance company paid us for the services you received on that date of service.
A Couple of Notes on Insurance Plans
- Most insurance companies offer several different insurance plans or subsidiaries. Thus, two patients with Blue Cross Blue Shield, for instance, may have completely different benefits, and therefore, completely different financial responsibilities. Some plans have no copays or deductibles; others may have a $10,000 deductible. Furthermore, some providers may not accept all insurance plans from a particular insurance. This is why it is crucial that you investigate the details of your specific plan.
- If your insurance plan offers an online patient portal, sign up for it! These resources typically enable you to:
- check your benefits,
- track your deductible,
- see which providers in your area accept your particular plan,
- track your claims, and
- compare claims to your receipts from the doctor’s office (if they don’t match up, you can then follow up on any discrepancies).
Tips for Choosing an Insurance Plan
Whether you’re shopping for your own insurance plan or going through the benefits selection process with your employer, choosing the right plan can seem like an overwhelming task. While we can’t tell you which specific plan to choose, the following questions should help you with the selection process.
Questions to Ask Potential Insurance Carriers
This is the monthly amount you pay for coverage. The lower it is, the higher your deductible will typically be. Plans with low premiums and high deductibles often are called “catastrophic” plans. Conversely, higher premium plans often feature lower deductibles, copays, and coinsurances.
This is the total amount you must pay each year before your insurance begins to pay. For example, if your deductible is $4,000, then you must pay $4,000 toward deductible-applicable services before your insurance will pay anything. If your deductible applies to PT services, then you may have to pay an estimate of anywhere from $75 to $120 per visit until you meet your deductible. Once you reach your deductible, your copay or coinsurance will then apply.
High copays are another common drawback to low-premium plans. Remember, the copay applies even after you have met your deductible, and the copay for specialist visits—including PT visits—can be as high as $80. So, if you anticipate a lot of office visits during this plan year, you will definitely want to factor the copay into your decision process.
As previously noted in this document, coinsurance is another version of cost-sharing. So, you’ll likely have to pay either a coinsurance or a copay. However, while copays are fixed amounts—and thus, are more predictable—coinsurances are percentages. Therefore, your financial responsibility varies based on how much your provider charges for the services rendered.
Some insurance plans (e.g., PPOs, HMOs, and EPOs) are limited to a certain network of providers. So, make sure you have a good selection of covered providers and facilities in your area. If you travel frequently or live in a rural area, you may want to choose a plan that has no network restrictions.
If your insurance plan requires you to obtain a referral before seeing a specialist (e.g., a physical therapist), and you fail to do so, the insurance company may deny coverage for services rendered. So, if you do not want to go through a primary care provider (e.g., your family physician) each time you want to see a specialist, make sure your plan does not require a referral (a.k.a. prescription) for specialist services.
In this case, “X” represents a specific type of service (e.g., physical therapy, occupational therapy, or chiropractic). Some plans place a limit on the number of covered visits per year (e.g., 20 visits), while others allow for unlimited visits. If you’re athletic, have chronic joint pain, or anticipate needing a joint replacement in the near future, you may not want any restrictions on the number of rehabilitative visits allowed.
Medicare only pays 80% of the cost of care, so many Medicare beneficiaries seek secondary insurances to pay the other 20%. However, even those plans often feature deductibles, copays, coinsurances, or visit limitations. Thus, we recommend posing all of the above-listed questions to any secondary insurances you are considering.
The Bottom Line
Higher-premium insurance plans are generally better for individuals who expect to receive medical care on a regular basis. Lower-premium plans will save those individuals money monthly, but those savings won’t make up for the cost-sharing portion.
The Self-Pay Option
If I don’t want to use my insurance, can I just pay for services myself?
The self-pay rate for all follow-up visits at Kinetic is $85. The initial evaluation visit for physical, occupational, or speech therapy is $120. Because an insured patient with a deductible may have to pay $85 or more for the same service, many insured patients ask if we can essentially “pretend” they are uninsured. However, if we contract with your insurance company, we are obligated to honor that contract—which means we must bill your insurance for services rendered. Some contracts also prohibit us from providing discounts or waiving patient financial responsibility (e.g., copays or coinsurances). That said, if we do not contract with your insurance, or if you have exhausted your benefits for the year, then you may be eligible to receive services on a cash-pay (i.e., self-pay) basis.
Questions about getting a massage in Greenville, NC. Contact Kinetic Physical Therapy today!


