Thoracic Outlet Syndrome
What is Thoracic Outlet Syndrome?
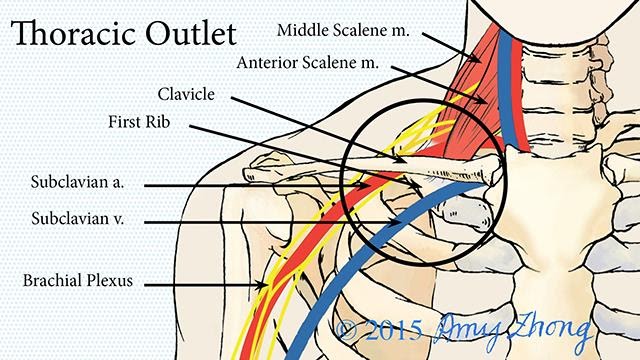
The thoracic outlet is an area at the base of the neck in between the space behind your collar bone and in front of your shoulder. This area is where the main highway of nerves, veins, and arteries that supply your shoulder and entire arm run. Thoracic outlet syndrome (TOS) is the name of a disorder that occurs when this area is compromised. TOS may occur with just the arteries or just the veins or just the nerves or a combination of all three. TOS that affects the nerves is called neurogenic thoracic outlet syndrome (nTOS), and it will be the main topic of later discussion here. The nTOS is by far the most common presentation of the disorder. However, a quick overview of all three:
Arterial TOS: Usually present from birth. Symptoms include coldness in the hands and arms and poor circulation.
Venous TOS: This occurs when the veins are blocked. This may be due to trauma or overuse overhead. Symptoms include swelling of the arm and enlarged veins in the neck and chest area
Neurogenic TOS: This occurs from trauma or a structural defect (such as an extra rib). Symptoms include hand and arm pain and weakness, coordination difficulty in the arm, numbness in the arm and hand.
What is Neurogenic Thoracic Outlet Syndrome?
Neurogenic Thoracic Outlet syndrome can be caused by several factors. Usually, it is caused by an extra rib in the neck, which people could be born with, which pushes up into the space that the nerves occupy. Trauma from car accidents or other high-speed collisions are also a big cause due to some muscles that become overactive after injury and pinch down on the nerves. An nTOS is defined by numbness and weakness in the shoulder and down the arm. These symptoms may also be symptoms of a nerve injury from the neck, so it is important to have a good assessment from your healthcare provider.
Symptoms of Thoracic Outlet Syndrome
As stated before the primary symptom of nTOS is numbness and tingling. The location can vary based on what part of the nerve is compressed, but it usually involves a part of the hand and elbow vs being the whole hand and whole arm. Weakness and clumsiness is also a common report due to the muscles being impacted by lack of nerve input. Regular headaches are also a common symptom due to the nature of the injury. All of these symptoms are exacerbated by using the arm, especially overhead.
How is Thoracic Outlet Syndrome Diagnosed?
This is tough to easily summarize. In the case of an extra rib, the diagnosis is easy to make off an x-ray. Otherwise, an nTOS diagnosis is complex because the typical imaging such as CT, ultrasound, and MRI aren’t reliable. The nerve compression usually occurs when the arm is moving and the nature of these imaging tests require that you sit still. EMG studies (studies in which nerve conduction is measured) are also unreliable for the same reasons. The EMG studies will typically show that the nerve has been injured but they don’t do a good job of showing where. The gold standard for diagnosing an nTOS involves putting an injectable muscle block into the muscles near the area. This block will relax the pressure on the compressing structures and result in the nerve being “freed” up.
How can a Physical Therapist Help with a Thoracic Outlet Syndrome?
A good physical therapist can help recognize nTOS and early recognition and treatment are vital to long term improvement. With proper early treatment, the compression on the nerves can be eased and the overactive neck/trunk muscles can be calmed down and stretched appropriately. The shoulder, elbow, and hand range of motion and strength can be maintained or even improved while the neural structures recover from the injury. Patients with an nTOS should NOT go by “No pain/no gain,” which may result in prolonging the injury or making it permanent. A good therapist will make improvements in posture and movement patterns to improve pain and function long term. However, despite our best efforts, some patients do not improve with therapy and we will work with your doctor to find the best treatment approach to suit your needs.





